Supported by an educational grant from BioWave.
Introduction
Data from the National Health Interview Survey and Centers for Disease Control and Prevention (CDC) report that in 2019, 20.4% of adults in the United States had chronic pain. 7.4% of adults had high-impact chronic pain (or 36.4% of all adults who had chronic pain) that has negatively impacted their function, mental health, employment, and quality of life (QoL) in the past three months.1 Women were more likely to experience chronic pain compared to men (21.7% vs. 19.0%), as well as higher incidence of high impact chronic pain (8.5% vs. 6.3%).1
These data reflect a significant social and socioeconomic burden to individuals afflicted with chronic pain. While chronic pain conditions are characterized by their type of pain pathophysiology—neuropathic, nociceptive, and centralized pain/central sensitization—individual outcomes are influenced by co-occurring psychosocial factors necessitating the application of an integrated and multimodal treatment approach that considers comorbidities, cognitive and emotional characteristics, social determinants of health, and functional impairment.2
Types of Pain
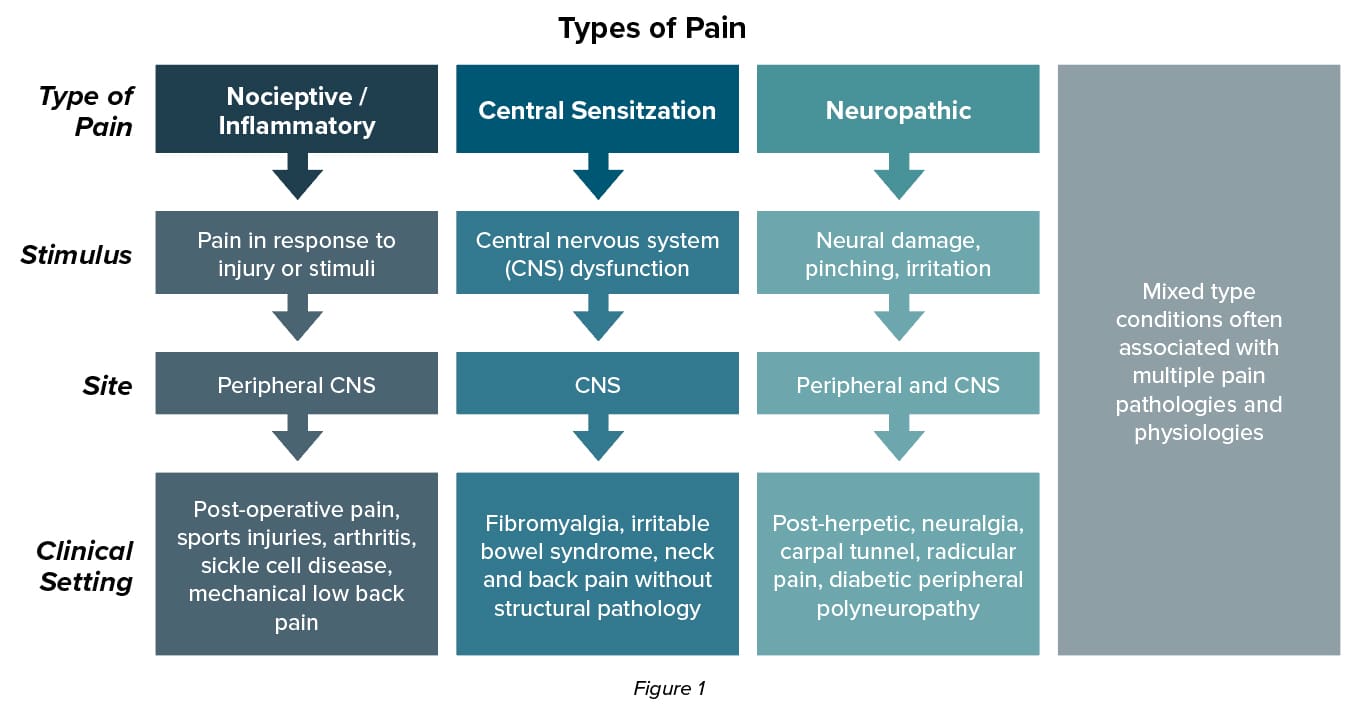 Pain is a complex biologic and psychologic phenomenon that is often poorly understood and inadequately managed by primary care providers because of insufficient education and training.3 A mechanism-based approach can be applied to the clinical assessment and management of pain.4 Nociceptive pain arises from actual or threatened damage to non-neural tissue and is caused by the activation of nociceptors. Central sensitization pain arises from altered nociceptors despite no clear evidence of active tissue damage causing the activation of peripheral nociceptors, or evidence for disease or lesion of the somatosensory system causing the pain. Neuropathic pain is caused by a lesion or disease of the somatosensory nervous system. Mixed type conditions are often associated with multiple pain pathologies and physiologies.
Pain is a complex biologic and psychologic phenomenon that is often poorly understood and inadequately managed by primary care providers because of insufficient education and training.3 A mechanism-based approach can be applied to the clinical assessment and management of pain.4 Nociceptive pain arises from actual or threatened damage to non-neural tissue and is caused by the activation of nociceptors. Central sensitization pain arises from altered nociceptors despite no clear evidence of active tissue damage causing the activation of peripheral nociceptors, or evidence for disease or lesion of the somatosensory system causing the pain. Neuropathic pain is caused by a lesion or disease of the somatosensory nervous system. Mixed type conditions are often associated with multiple pain pathologies and physiologies.
Understanding the basic concepts of pain pathophysiology can inform an effective pain management strategy because different pain interventions and pharmacotherapies target different pain mechanisms. Traditional treatments for inflammatory nociceptive pain such as rheumatic diseases, gout, osteoarthritis, and neck and back pain with underlying structural pathology include nonsteroidal anti-inflammatories (NSAIDs), opioids, or topical agents such as lidocaine and capsaicin.6 Treatment options for neuropathic pain may include gabapentinoids, serotonin norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants.6 Figure 1 outlines the different subtypes of pain, the stimulus, the site of pain processing, and the clinical setting in which clinicians may encounter these different types of pain.5
The peripheral nervous system (PNS) is an integral part of the body’s communication with the environment. 7,8 Touch, proprioception, temperature, and nociception influence our perception of the world.8,9 Pathological persistence of nociception from the PNS or peripheral nerve dysfunction can alter and amplify activity within pain pathways. Biochemical mediators drive pathophysiological sequences that cause changes in the cell bodies on the somatosensory neurons which in turn lead to central changes that clinically manifest as ongoing pain, allodynia, hyperalgesia, hypersensitivity, or loss of movement or function.10-13
Addressing Unmet Needs in Pain Management
Unmet needs remain in the management of chronic pain and each medication is associated with related adverse events. NSAIDs may not be suitable for older adults or patients with gastrointestinal or renal complications.6 Opioids can lead to dependence and substance use. These safety concerns are magnified by CDC reports concluding that 25.8% of patients with chronic pain are between 45-64 years of age and 30.8% of patients with chronic pain are 65 years and older.1 Targeting the PNS as part of the chronic pain management strategy may include physical therapy, pharmacological management, thermal or chemical ablative therapy, and/or neurostimulation such as spinal cord stimulation (SCS). Interventional pain specialists may also use peripheral nerve blocks using local anesthetics.8,14
Noninvasive bioelectronic medicine describes the use of neurostimulation to modify the response of nerve tissue to reduce pain. Bioelectronic medicine offers the ability to employ electrical, magnetic, optical, and ultrasound technologies to deliver targeted, personalized therapy and eliminate the need for medication, offering new options to patients with chronic pain that remains unresolved with traditional pharmacological treatment.10
In order for noninvasive bioelectronic technologies to have sustained influence on the PNS, the high-frequency electric field must be able to bypass the skin, using a low-frequency electric field (1 to 180 Hz) to halt the propagation of action potentials that lead to the hyperpolarization. This is achieved by combining two sinusoidal high-frequency signals that penetrate deep tissue and promote multiplication of the signals.10
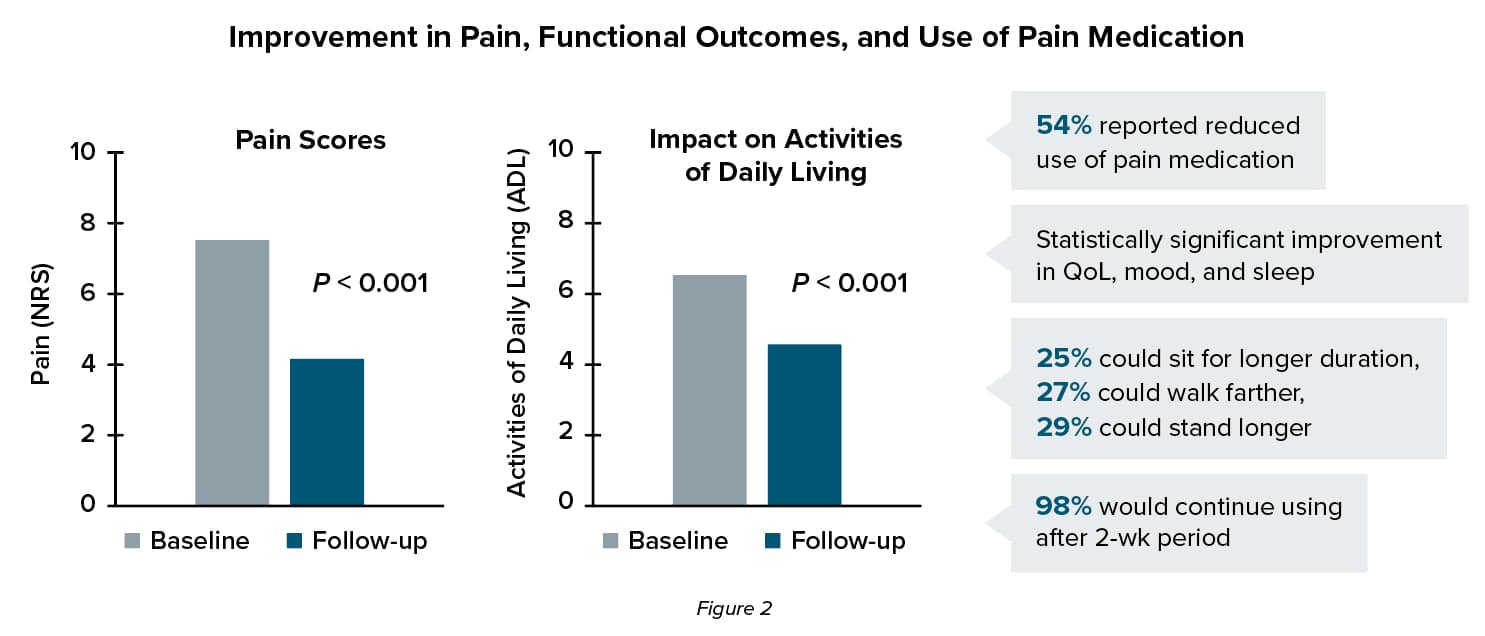
An open-label pilot study examined the impact of noninvasive high-frequency peripheral nerve fiber stimulation on pain intensity, activities of daily living, functional capacity, and medication consumption in a cohort of 463 individuals with chronic pain over a period of two weeks.10 Patients enrolled in the study presented with a chronic lower-back, neck, upper- or lower-limb pain for more than three months who attended a Veterans Affairs (VA) medical center, pain clinic or orthopedic clinic between February 2019 and July 2020. Patient characteristics included:10
- Most patients had chronic pain alone, 21% reporting acute pain over 2-week period
- 81% of patients reported chronic back pain and chronic neck pain
- Only a small percentage of participants were able to report whether their pain was nociceptive or neuropathic.
 Enrolled patients were trained in the use of the BioWave-HOME device and on the correct position of the skin electrodes. Stimulation was delivered via high-frequency sinusoidal alternating current signals at 3858 and 3980 Hz. B-set electrodes were used for treating the origin of pain and most proximal location of pain to the origin. E-set electrodes were placed over a single location of pain and over a bony prominence that was comfortable to receive stimulation.10
Enrolled patients were trained in the use of the BioWave-HOME device and on the correct position of the skin electrodes. Stimulation was delivered via high-frequency sinusoidal alternating current signals at 3858 and 3980 Hz. B-set electrodes were used for treating the origin of pain and most proximal location of pain to the origin. E-set electrodes were placed over a single location of pain and over a bony prominence that was comfortable to receive stimulation.10
The key findings suggest that the noninvasive high-frequency neuromodulation can significantly improve pain intensity and activities of daily living (ADLs). Improvements were also seen in secondary outcomes including QoL (94%), mood (29%), and sleep (33%).
Authors concluded that the pilot survey highlighted the potential role of a novel bioelectronic technique to manage pain and improve ADL. Further research will examine longer-term effects of this treatment option.10
Partnering with Patients
As with all treatment strategies, shared decision-making plays an important role in treatment decisions. Patient education about the value of a multimodal treatment strategy is an essential element of health literacy so patients can be active participants in their pain care. Additionally, establishing treatment goals and engaging patients in treatment decision-making early, provides the opportunity to utilize peripheral neurostimulation as a viable option when value can be seen and not withheld as salvage treatment. An active clinician-patient partnership centered around participation, engagement, and collaboration fosters greater patient satisfaction, improved patient adherence, and ultimately optimal pain management outcomes.14
References
- Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic Pain and High-impact Chronic Pain Among U.S. Adults, 2019. NCHS Data Brief, No. 390. https://www.cdc.gov/nchs/products/databriefs/db390.htm. Published November 2020. Accessed July 21, 2021.
- Clauw DJ, Essex MN, Pitman V, Jones KD. Reframing chronic pain as a disease, not a symptom: rationale and implications for pain management. Postgrad Med. 2019;131(3):185-198.
- Stanos S, Brodsky M, Argoff C, et al. Rethinking chronic pain in a primary care setting. Postgrad Med. 2016;128(5):502-515.
- Chimenti RL, Frey-Law LA, Sluka KA. A mechanism-based approach to physical therapist management of pain. Phys Ther. 2018;98(5):302-314.
- Patapoutian A, Tate S, Woolf C. Transient receptor potential channels: targeting pain at the source. Nat Rev Drug Discov. 2009;8(1):55-68.
- Bates D, Schultheis BC, Hanes MC, et al. A comprehensive algorithm for management of neurpathic pain. Pain Med. 2019;20(Suppl1):S2-S12.
- Kiernan JA, Barr Ml, Rajakumar N. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10th Philadelphia: Wolters Kluwer Lippincott Williams & Wilkins; 2013.
- Deer TR, Naidu R, Strand N, et al. A review of the bioelectronic implications of stimulation of the peripheral nervous system for chronic pain conditions. Bioelectron Med. 2020;6:9.
- Benarroch EE, Cutsforth-Gregory KK, Flemming KD. Mayo Clinic Medical Neurosciences: Organized by Neurologic System and Level. 6th Oxford University Press; 2017.
- Hegarty DA, Bretherton B. An open-label pilot study investigating noninvasive high-frequency peripheral nerve fiber stimulation in chronic pain. Pain Pract. 2020 Dec 23. [Epub ahead of print].
- Gangadharan V, Kuner R. Pain hypersensitivity mechanisms at a glance. Dis Model Mech. 2013;6:889-895.
- Schaible H-G, Ebersberger A, Natura G. Update on peripheral mechanisms of pain: beyond prostaglandins and cytokines. Arthritis Res Ther. 2011;13:210.
- Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87-107.
- Martin LR, Williams SL, Haskard KB, DeMatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189-199.
